Breakthrough research in the stem cell field in 2016
December 30, 2016 Source: Bio Valley
Window._bd_share_config={ "common":{ "bdSnsKey":{ },"bdText":"","bdMini":"2","bdMiniList":false,"bdPic":"","bdStyle":" 0","bdSize":"16"},"share":{ }};with(document)0[(getElementsByTagName('head')[0]||body).appendChild(createElement('script')) .src='http://bdimg.share.baidu.com/static/api/js/share.js?v=89860593.js?cdnversion='+~(-new Date()/36e5)];Doi: 10.1161/STROKEAHA.116.012995
Patients with a stroke can significantly improve their speech ability, physical strength, and mobility by undergoing treatment with stem cells injected into the brain. Some of these patients are even able to walk again.
The success of this clinical trial means that we underestimate the brain's ability to heal itself, and perhaps one day therapy will restore the brain's function.
"A 71-year-old woman can only move her left thumb before treatment begins," said Gary Steinberg, a psychologist at Stanford University, who is the lead researcher at the study. "Now she can walk and raise her hand over her head."
This is the second clinical trial to restore brain function by injecting stem cells into the brain. A similar clinical trial in the UK last year was also successful.

[2] Stem Cells Transl Med: Stem Cell Therapy from Cat to Human
Doi:10.5966/sctm.2015-0127
When the kitten Bob came to the veterinary hospital at the University of California, Davis, it had already used up its nine lives; due to the pain of oral inflammation, Bob had already pulled out all the teeth and tried to be called this cat. In the fight against chronic gingivitis (FCGS), Bob entered a clinical trial with a new type of stem cell therapy. Bob was lucky enough to enter this clinical trial with other kittens. The trial was very successful and Bob was reborn.
The researchers published the results of this study in Stem Cells Translational Medicine; the researchers used stem cell therapy for the first time to successfully and effectively treat chronic gingivitis in cats; when the researcher Arzi witnessed many treatments After a cat with chronic gingivitis and losing all its teeth, he opened a clinical trial to treat cats. Chronic gingivitis is a difficult disease to treat. Researchers often see some cats. Traditional treatments did not respond, so they decided to use stem cell therapy to try; first they used the body's own fat-derived stem cells to process stem cells and conduct characterization, and then treat the treated stem cells to cats. Intravenous injections reduce the inflammatory performance of the cat's body and promote tissue regeneration; the researchers also identified a useful biomarker that can help determine if a cat responds to stem cell therapy.
[3] Sci Rep: Editing stem cell therapy or treating blindness
Doi:10.1038/srep19969
Recently, in a research paper published in the international journal Scientific Reports, researchers from Columbia University and others used CRISPR/Cas9 gene editing technology to successfully correct gene mutations in the stem cells of patients. The relevant research results may be late. The development of individualized treatments for eye diseases offers new clues.
Researcher Alexander Bassuk said that our goal is to repair the degenerative retina in the eyes of patients with X-linked retinitis pigmentosa (XLRP) disease. CRISPR/Cas9 is an accurate gene editing technique that can effectively correct damage. A single DNA change in the RPGR gene, and more importantly, the modified tissue is derived from the patient's own stem cells, which may be transplanted without the use of harmful drugs to inhibit tissue rejection.

[4] Top-level journals are concurrency: stem cells cure type I diabetes
In 2008, an estimated 347 million people worldwide have diabetes. The prevalence rate is still on the rise, especially in low- and middle-income countries. A total of approximately 1.5 million people died directly from the disease in 2012, with more than 80% of deaths occurring in low- and middle-income countries. According to WHO projections, diabetes will be the seventh leading cause of death by 2030. Over time, high blood sugar can seriously damage the body's major organ systems, causing heart disease, stroke, nerve damage, kidney failure, blindness, impotence, and infections that may cause amputation.
There are two main forms of diabetes. People with type 1 diabetes usually cannot secrete insulin themselves, so insulin needs to be injected to sustain life. Type II diabetes accounts for about 90% of the total number of cases of diabetes. Patients usually produce insulin on their own, but they cannot produce enough insulin or use it properly.
For most patients with type 1 diabetes, daily injections of insulin on a daily basis are the primary means of controlling blood sugar. There are also some patients who do not receive daily insulin injections and have received islet transplantation. This treatment is currently mainly restricted by two aspects: there is not enough lifetime rejection of islet donors and islet receptors.
[5] Stem cells for liver disease! Belgian cell therapy company Promethera plans IPO to advance HepaStem clinical development
Original source : Promethera plans IPO to bankroll pipeline of liver disease cell therapies
In the past few years, Belgian stem cell treatment company Promethera Biosciences has been reported by the media as an IPO. And recently, the company has finally put the IPO on the agenda. The company plans to raise 40 million euros (about $45 million) to fund the clinical advancement of its pipeline assets. Promethera's lead candidate HepaStem is a stem cell therapy, an allogeneic adult liver-derived progenitor cell, extracted from the donor's liver, processed and reconstituted into an injectable product, considered to have The potential to treat a variety of liver diseases.
Promethera has extensively tested HepaStem in patients with rare disease urea cycle disorders (UCD), and current Phase I/II clinical trials are ongoing. According to the company's statement, the IPO raised 30 million to 40 million euros will help to continue the clinical development of HepaStem treatment of UCD, while giving the company the opportunity to expand its strategic ambitions. In particular, since John Tchelingerian took over as CEO last year, the company has consistently signaled the expansion of HepaStem's clinical development indications.
[6] Neurology: Stem cell therapy for frozen human disease may be safe
DOI: 10.1212/WNL.0000000000002889
A phase II clinical trial of patients with amyotrophic lateral sclerosis (ALS) has shown that implantation of human stem cells into the spinal cord may be safe. The study was published online June 29, 2016 in the medical journal Neurology of the American Academy of Neurology. Although the study was not designed to determine whether treatment was effective, the researchers noted that treatment did not slow the progression of the disease.
ALS is a disease in which the motor neurons in the brain and spinal cord undergo progressive degeneration, also known as gradual freezing. The patient will gradually lose control of the muscles, including breathing and swallowing, and eventually die. There are currently no therapies that can stop the development of this disease.
“Although there are two serious complications associated with treatment, the level of acceptable risk for treating ALS patients is relatively high compared to more benign diseases.†Member of the American Academy of Neurology, Professor of Neurology, Emory University School of Medicine Dr. Jonathan D. Glass said.
The study was conducted in 3 university hospitals with 15 ALS patients involved. Initial ALS symptoms in all participants were within two years. Participants were divided into 5 treatment groups, and the dose of stem cells received was gradually increased. The trial was unblinded, meaning that participants knew they were receiving active stem cell therapy.
[7] Depth analysis of the mechanism of action between immune cells and stem cells to facilitate the development of stem cell regeneration therapy
News Reader: Immune Cell–Stem Cell Cooperation
We may think that we are static creatures, but in fact our cells are in constant flow, the outer skin of the body's skin and intestines is replaced every few weeks, and the red blood cells are circulated in the body before being replaced. About 100 days, while liver and fat cells tend to live longer, each liver cell can survive for more than 1 year, and fat cells have an average lifespan of 10 years. These cells are repeatedly replaced and updated during our lifetime. About half of the heart cells in an individual's normal life are replaced; when healthy tissue is lost due to injury, the new cells will repair the damage, so what is the biological process of normal cell renewal and organ balance? What controls the damage repair of the body after the body is damaged? A series of questions are the key issues to be studied in the field of regenerative medicine research.
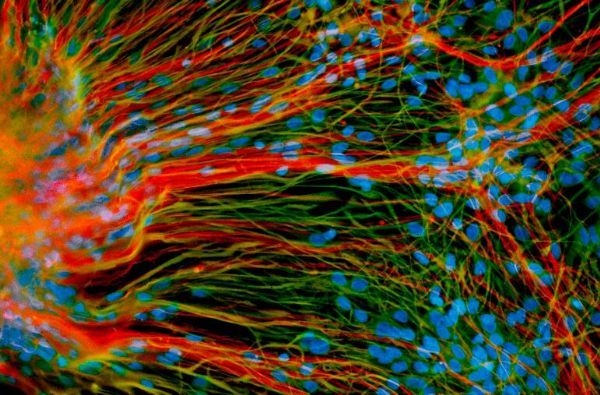
For nearly half a century, scientists have known that stem cells are vital members of our body. Stem cells can self-renew to maintain their constant number and differentiate into specific types of cells that assemble and form the tissues and organs of the body. Organs and tissues are important for body stress or repair after injury; the researchers believe that the ultimate goal of regenerative medicine research is to use stem cell regenerative potential to treat or cure a variety of diseases. Although current researchers have made great progress in understanding the potential of these pluripotent stem cells, in reality we are far from being able to cure diseases. One reason is that research does not fully consider and reveal changes in the biological environment around stem cells. .

[8] Nat Commun: New research successfully applied stem cell therapy to delay progression of Huntington's disease in mice
Doi:10.1038/ncomms11758
Recently, researchers have successfully used healthy human brain cells to delay the progression of disease in the mouse model of Huntington's disease and alleviate the symptoms of the disease. The findings are published in the international academic journal Nature Communication, a new approach to the treatment of Huntington's disease.
Huntington's disease is a hereditary neurodegenerative disease caused primarily by damage to medium-sized spiny neurons responsible for motor control. Patients with this disease may have disorders of movement, cognitive decline, and depression, and there is still no effective way to treat or delay the disease.
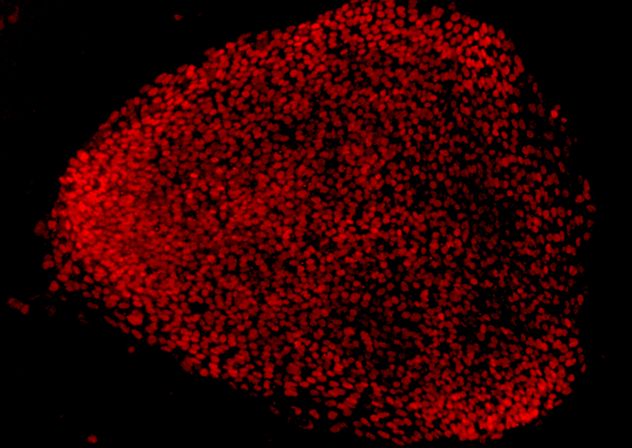
In this latest study, the researchers used embryonic stem cells and glial progenitors obtained from brain tissue to perform a series of experiments in which the isolated cells were implanted into the striatum of the Huntington mouse model, and previous studies. The results were consistent. The researchers observed that astrocytes differentiated from glial progenitor cells gradually replaced the original glial cells, so that the mice had both their own neuronal cells and healthy human glial cells. . Studies have shown that human glial cells can maintain the health of the mouse's neuronal cells, and can also prolong the survival of the mice, the behavior, memory and exercise ability of the mice also performed better.
[9] Nat Commun: Stem Cell Therapy for Diabetes Mellitus Mature Scientists have achieved the use of patient tissue to obtain beta cells
Doi:10.1038/ncomms11463
Recently, researchers from the University of Washington School of Medicine and Harvard University used induced pluripotent stem cells formed by tissue from patients with type 1 diabetes to obtain beta cells with insulin-secreting function, finding a new potential method for treating diabetes. Type 1 diabetes patients are unable to synthesize insulin themselves, so regular injections of insulin are needed to help control blood sugar. This latest finding shows that the individualized treatment of diabetes has seen the dawn.
The relevant research results are published in the international academic journal Nature Communication.
Prior to this study, researchers used induced pluripotent stem cells formed by normal human tissue to differentiate into beta cells, and there has been doubt about whether beta cells can be obtained from tissues of diabetic patients, so they asked this question in the study. Investigated. The researchers used the induced pluripotent stem cells formed by the skin cells of diabetic patients to differentiate into β-cells. These patient-derived beta cells are capable of expressing the molecular markers of beta cells and respond to glucose in both in vitro and in vivo conditions, while in beta models these beta cells prevent alloxan-induced diabetes and fight against diabetes drugs. Generate a response.

[10] Cell Metab: Scientists find the "life gate" of human pluripotent stem cells to help solve the problem of tumor formation in stem cells
Doi:10.1016/j.cmet.2016.03.001
Recently, the international academic journal Cell Metabolism published a new research progress in the Keio University School of Medicine in Japan. They found that human pluripotent stem cells (hPSCs) cannot survive in the absence of glucose and glutamine, due to the special presence of hPSC. Gene expression patterns, therefore, cannot effectively utilize pyruvate. This study is important for eliminating undifferentiated stem cells remaining during stem cell therapy and preventing tumor formation.
Previous studies have found that human pluripotent stem cells rely on aerobic glycolysis to produce ATP, but the main energy source and importance of oxidative phosphorylation during ATP synthesis has not been fully elucidated.
[11] Stem Cells: Scientists find ways to improve the therapeutic potential of stem cells
DOI: 10.1002/stem.2510
Stem cells have great hopes for translational medicine. The key to the treatment of many different diseases is stem cell therapy, but scientists who grow and expand stem cells in the laboratory often encounter problems with stem cells losing their therapeutic potential. In a new study, researchers have conducted in-depth research on cellular mechanisms that help develop targeted methods to help maintain the characteristics of stem cells, human mesenchymal stem cells, and make stem cells more clinically useful.
"We found that mitochondria communicate with changes in cells and perform metabolic reconfiguration to maintain the original hMSC characteristics," said author Dr. Teng Ma. "These findings suggest that mitochondria and metabolism play an important role in maintaining stem cell characteristics during hMSC culture."
[12]Circulation Res: The mechanism of cardiac stem cell therapy remains a mystery
Doi:10.1161/CIRCRESAHA.115.307647
In numerous clinical trials, scientists have injected different types of progenitor cells into the patient's body to help treat the damaged heart. In some cases, the patient does have better heart function, but how is it caused? There has always been a disagreement between the scientists on this issue. According to a new study of rats, the researchers found that the progenitor cells injected into the body did not itself produce new cardiomyocytes by proliferation, resulting in improved cardiac function. The results of the study were published online in the journal Circulation Research on February 2, 2016. The paper titled "Long-Term Outcome of Administration of c-kitPOS Cardiac Progenitor Cells After Acute Myocardial Infarction: Transplanted Cells Do Not Become Cardiomyocytes, but Structural and Functional Improvement and Proliferation of Endogenous Cells Persist for At Least One Yearâ€.
"These cells don't turn into adult cardiomyocytes," says Roberto Bolli, co-author and researcher at the University of Louisville University's Heart Cell Therapy. "Therefore, the mechanism is clearly a paracrine effect, that is, these cells release a certain The 'substance' that makes the heart better. The most important question is 'What is this substance?
• Warmed humidified air is better than cold, dry gases even in short cases.
When a patient`s trachea is intubated or a supraglottic airway device is placed in situ, the normal warming, humidifying and filtering functions of the upper airways are bypassed. Hence, gas delivered to the patient needs to be artificially conditioned to replace these lost functions Heat and moisture exchangers (HMEs) are intended to conserve a portion of the patient`s exhaled heat and moisture, and condition inspired gas by warming and humidifying it. Breathing system filters are intended to reduce the transmission of microbes and other particulate matter in breathing systems.
Devices that contain both filters and HME are called Heat Moisture Exchanger Filters (HMEFs). It is not ideal to distinguish these two common filters with "static" and "folds", because these two types of filters rely on electrostatic charge to a certain extent to keep the particles in the filter material, two types All materials can be folded. The main difference between the two types is the density of the fibers. For "electrostatic" filter materials, the density of the fibers is relatively low, and the electrostatic charge (fiber or triboelectric charge) on the fibers is high. For "pleated" filters, the density of the fibers is high: this leads to increased resistance to gas flow; the pleated material increases the surface area, thereby reducing the resistance. This type of filter is also called "hydrophobic" (because the surface of the filter material repels water) or "mechanical". In this review, the terms "electrostatic" and "pleat" will be used to distinguish these two types of filters.
Disposable Breathing Filter \Airway Management
Zhejiang Haisheng Medical Device Co., Ltd , https://www.hisernmedical.com